The role of investigative testing in general practice
By Dr David Deam
Published March 2025
General practitioners are pivotal in the early detection and risk stratification of cardiac disease. As the initial point of contact for patients presenting with potential cardiovascular symptoms, including palpitations, dizziness or uncontrolled hypertension, GPs are uniquely positioned to initiate targeted investigations. This proactive approach facilitates timely risk assessment, expedites specialist referral pathways and optimises patient management while awaiting cardiology consultation.
In this article, Melbourne cardiologist and Founder and Medical Director of CardioScan, Associate Professor Harry G Mond, and Clinical Labs chemical pathologist Dr David Deam explore key investigative tests that GPs can order for patients presenting with cardiac symptoms in general practice.
Biochemical Investigations: Useful investigations for diagnosing and managing heart disease
By Dr David Deam
Assessing overall cardiovascular disease (CVD) risk
Assessing CVD risk using the Australian guideline and calculator (cvdcheck.org.au) is a useful first step when investigating or reviewing patients for possible increased risk of heart disease. This is appropriate for people without known CVD aged 45–79 years, diabetic patients 35-79 years and First Nations people aged 30–79 years. The tool provides an estimated 5-year CVD risk ranking of:
- High (≥10%)
- Intermediate (5% to <10%)
- Low (<5%)
Biochemical investigations
A wide range of biochemical tests can be useful in the assessment and treatment of heart disease. Some of these have been summarised in Figure 1.
The suggested investigations below are not exhaustive and should be considered within the clinical context.
Chest Pain
Investigating chest pain is best done in a setting where resuscitation facilities are available. Initial investigations include a troponin measurement and a 12-lead resting electrocardiograph (ECG). These tests are usually then repeated after a period of several hours, depending on local protocols.
Hypertension (BP)
Besides repeated blood pressure measurements or a 24-hour ambulatory recording, investigations for secondary causes of hypertension can also be appropriate. These are best done before the patient commences treatment.Typical tests include investigations for:
- Adrenal causes
- Hyperaldosteronism (renin-aldosterone ratio)
- Pheochromocytoma (urine catecholamine or metabolites)
- Cushing’s syndrome (cortisol)
- Liver disease (liver function tests)
- Renal disease (urea and electrolytes)
- Thyroid disorders (thyroid function tests)
Heart Failure
Patients with suspected or known heart failure can now be investigated with a B-type natriuretic peptide (BNP) measurement. A significant new MBS item for NT-proBNP or BNP testing, item 66829, was added to the Medicare Benefits Schedule on 1 November 2024. This new item broadens the range of clinical situations in which NT-proBNP or BNP testing can be ordered.
Cardiac Arrhythmias and Palpitations
The initial investigation for arrhythmias and palpitations is a resting 12-lead ECG, followed by 24-hour ambulatory ECG monitoring (Holter study). Biochemical testing for electrolyte imbalances (potassium, calcium, magnesium), digoxin levels and thyroid disorders can also be useful.
Atherosclerosis
Serum lipids (cholesterol, triglycerides, HDL cholesterol, LDL cholesterol and non-HDL cholesterol) have an important association with atherosclerosis and measuring levels is useful in diagnosing and managing lipid disorders. Some more specialised investigations, such as apolipoprotein (a) and high-sensitivity C-reactive protein (hs-CRP), can be helpful in selected patients.
Figure 1. Useful investigations for diagnosing and managing heart disease
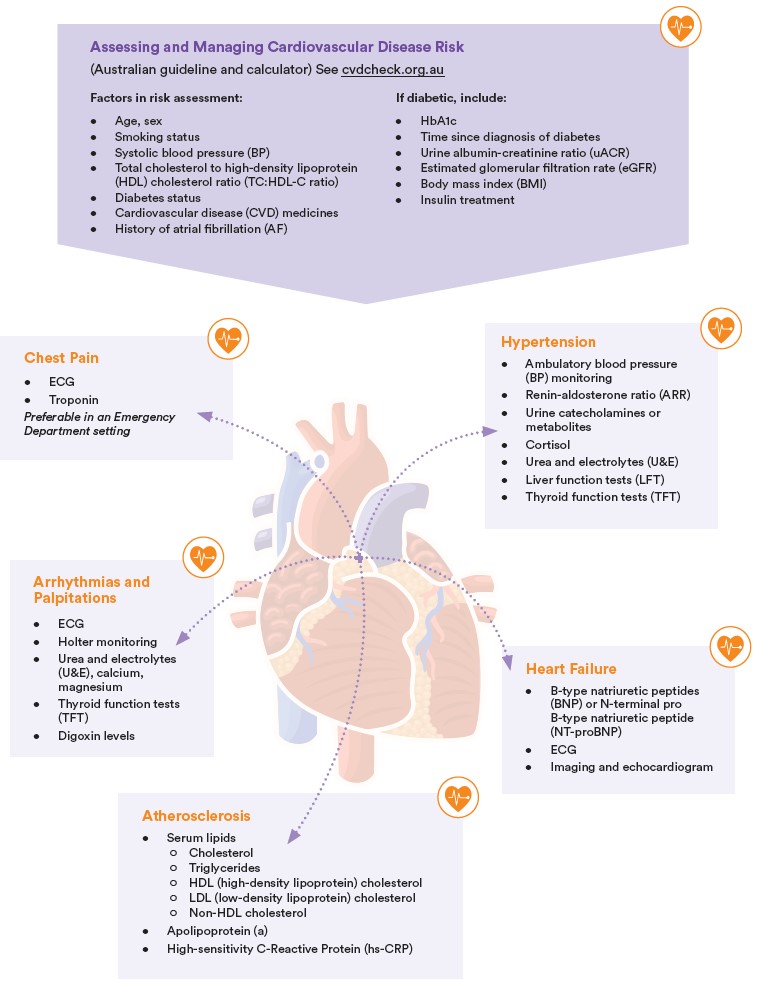
This figure was created by Dr David Deam, Clinical Labs Chemical Pathologist.
Cardiovascular Investigations: The value of the 12-Lead ECG, Holter monitoring and ambulatory blood pressure monitoring in general practice
By Associate Professor Harry G Mond
In recent years, technological advances have enabled the widespread use of a number of cardiovascular investigations by general practitioners, specialist physicians and public and private hospitals to exclude or identify cardiac arrhythmias and occult hypertension. These include the resting 12-lead electrocardiograph (ECG), the 24-hour or multi-day Holter monitor (ambulatory ECG monitor) and the 24-hour ambulatory blood pressure monitor. For each investigation, the available recording equipment is reliable and robust, with results available to the referring doctor or hospital within a timely manner (ECG in 4 hours) of the procedure being completed. This has allowed general practitioners to immediately initiate appropriate and, in some instances, life-saving treatment, bypassing long waiting times for specialist or hospital investigations.
Resting 12-lead ECG
In 1905, Nobel laureate Willem Einthoven (Physiology/Medicine, 1924) first described both normal and abnormal ECGs in human subjects. The bulky, primitive equipment eventually became the primary investigative tool for any cardiology patient visiting a physician. Now, 120 years later, despite the vast improvements in cardiological investigations, the resting 12-lead ECG—greatly improved technologically—remains the first cardiology investigation performed during a consultation or hospital visit. Modern recording equipment is small, portable and battery-operated. Initially, tracings were recorded on heatsensitive or photographic paper, but today, recordings can be sent electronically, allowing immediate reporting and transfer to the requesting physician.
In recent years, there have been expanding indications for the 12-lead ECG. These include:
- Heart health
- Pre-operative evaluation
- Palpitations/skipped beats
- Bradycardia
- Chest pain
- Dizziness and syncope
- Familial sudden death syndromes, including athletes
- Hypertension
- Cardiomyopathy
- Dyspnoea
- Stroke
- Pacemaker evaluation
Holter (ambulatory ECG) monitoring
The resting 12-lead ECG provides only a 10-second “snapshot” of the heart’s electrical activity. For a patient with intermittent palpitations and dizziness, longer recordings are essential. In the 1950s, Norman Holter, a Montana physicist, designed a 39 kg monitor and radio transmitter to record the ECG in real time. By the 1960s, magnetic tape recorders and later cassettes allowed for the development of smaller portable recorders. With further improvements in 24-hour and multi-day ambulatory ECG monitoring, our understanding of the natural history of arrhythmias has greatly improved, resulting in an expanding list of indications for both the standard 12-lead ECG and a broad range of ambulatory ECG monitoring devices. These include:
- Cardiac palpitations. This is by far the most common indication for ambulatory ECG monitoring. Generally, a 24-hour monitor is performed even when symptoms are infrequent. Two and three channel, 24-hour and multi-day recordings can be diagnostic for supraventricular and ventricular arrhythmias.
- Unexplained syncope or dizziness. When these symptoms are frequent, such as daily dizziness, 24-hour monitoring is very useful and is generally the initial investigation, even with relatively infrequent episodes. When the symptoms are less frequent, multiday monitoring is recommended.
- Suspected slow heart rhythms. 24-hour ambulatory monitoring remains the most important investigation in the evaluation of symptomatic patients who are being assessed for pacemaker implantation.
- Hereditary ‘‘electrical” abnormalities. This diverse group involves a number of hereditary abnormalities associated with cardiac arrhythmias. The most common is Wolff-Parkinson-White syndrome, manifested by an accessory pathway, ventricular pre-excitation and atrioventricular re-entrant tachycardia. The value of ambulatory ECG monitoring is to record arrhythmias, particularly in symptomatic patients.
- Evaluating an abnormal ECG with ectopy and heart block. This is a particularly important indication for 24-hour ambulatory monitoring to determine the significance of an abnormal ECG finding.
- Cryptogenic stroke evaluation to document paroxysmal atrial fibrillation. The neurologic finding that atrial fibrillation can lead to cryptogenic stroke was the major stimulus for the development of multi-day and long-term ambulatory monitoring technologies. Long-term monitoring includes implantable loop recorders.
- Evaluation of success of either antiarrhythmic or ablative therapy. 24-hour or multi-day ambulatory monitoring is valuable for recording breakthrough arrhythmias. On a long-term basis, non-prescription, single channel monitors such as smartwatches may also be used, although these items are of limited value in the initial diagnosis.
- Paediatric ambulatory monitoring. This is a special subgroup requiring paediatric equipment if available. Often, multi-day monitoring is necessary, particularly if the patient is unable to document symptoms.
- Following acute myocardial infarction. Patients who experienced atrial and ventricular arrhythmias or atrio-ventricular block during the acute phase of the infarction may require multi-day ambulatory monitoring following discharge.
- Potentially lethal arrhythmias with congestive and hypertrophic cardiomyopathy. Patients with cardiomyopathies require ambulatory monitoring to determine if antiarrhythmic or interventional therapy is necessary.
- Monitoring cardiac implantable electronic device therapy. Modern implanted cardiac pacemakers and cardioverter-defibrillators have inbuilt telemetric monitoring to determine usage and arrhythmia detection. Ambulatory monitoring is important in symptomatic patients where there is no documented telemetered abnormality.
- Chest pain or dyspnoea thought to be associated with arrhythmias or ST changes. These are unusual, but nevertheless valuable indications for ambulatory monitoring. Occasionally, cardiac arrhythmias, including both bradyarrhythmias and tachyarrhythmias, are the cause of dyspnoea. Patients with anginal-like chest pain may demonstrate marked ST elevation on the ECG due to coronary artery spasm, called Prinzmetal angina.
Monitoring hardware
The most frequently used hardware is the 5-lead, 3-channel, 24-hour Holter monitor. Current models are small, light, battery operated and feature a patientactuated button for event recording. Multi-day recorders may be 1 to 3 channel, and because of artefacts seen with long-term monitoring, company-specific chest wall patches have been designed to which the monitor is attached. Two- and three-channel monitors are preferred over single-channel models.
Data analysis and report
Once the patient has completed monitoring, the equipment is returned to the Australian Clinical Labs laboratory, where the recorded data is retrieved from the memory card and sent to CardioScan, responsible for analysing the raw data. A report is provided and confirmed by an experienced CardioScan cardiologist, then sent to the referring doctor. The report includes a summary of the 24 hour or multi-day study, significant events and the conclusion. Although therapeutic options are not provided, a CardioScan cardiologist is available to explain the results if necessary. For the requesting physician, there is a minimal knowledge requirement for competency in interpreting ambulatory ECG monitoring reports.
Ambulatory blood pressure monitoring
Every doctor understands the importance of detecting and treating occult hypertension at all ages. In recent years, ambulatory blood pressure monitoring has become a recognised and reliable method for confirming hypertension. The National Heart Foundation of Australia, in its summary of recommendations, states that “ambulatory blood pressure monitoring be offered to patients with a blood pressure ≥ 140/90 in order to confirm the blood pressure level”.1 Indeed, guidelines from the United States, Britain and Europe recommend ambulatory blood pressure monitoring as a cost effective diagnostic tool for all patients with suspected hypertension. Sophisticated, automated, 24 hour ambulatory blood pressure monitors are now available, and like all investigations, the results depend on the quality of the recordings and their interpretation in the clinical setting.
Ambulatory blood pressure monitoring should cover close to a 24-hour period, with >70% of recordings being valid. Recordings are usually performed every 30 minutes during the day and at least hourly overnight. It is recommended that at least 14 recordings be performed during the daytime period.1 However, monitoring is not without its difficulties, as cuff inflation can sometimes be painful and uncomfortable, leading to the patient removing the monitor overnight because of difficulty sleeping. Invalid recordings may occur if the cuff is not appropriately attached, is removed and reattached by the patient or if there is a leak or obstruction in the tubing. Movement during the recording may also result in an invalid measurement. In these situations, measurements are often automatically repeated, and there may still be enough data (> 14 recordings) to establish a diagnosis, even if the percentage of valid measurements is < 70%. This is important, as the vast majority of patients who experience discomfort during the study will not be prepared to have the study repeated.
The interpretation of results requires a clinical assessment, taking into consideration well-established risk factors for cardiac disease. Consequently, the referring doctor can modify the report conclusions to suit the patient’s individual circumstances, such as a young diabetic with renal disease who requires optimal control. The referring doctor, and not the reporting physician, should review the patient diary with the patient.
Table 1: Accepted normal limits for ambulatory blood pressure recordings.
| Ambulatory Blood Pressure | Systolic (mmHg) | Diastolic (mmHg) |
|---|---|---|
| Over 24 hours | ≥ 130 | ≥ 80 |
| Awake (daytime) | ≥ 135 | ≥ 85 |
| Asleep (night-time) | ≥ 120 | ≥ 70 |
| % allowed above limit | < 25% | < 25% |
Table 2: Guidelines on severity of recorded pressures (Clinical and not 24-hour ambulatory recordings).1
| Diagnostic Category | Systolic mmHg | Diastolic mmHg |
|---|---|---|
| Optimal | < 120 | < 80 |
| Normal | 120-129 | 80-84 |
| High normal | 130-139 | 85-89 |
| Isolated systolic | > 140 | < 90 |
| Grade 1: Mild | 140-159 | 90-99 |
| Grade 2: Moderate | 160-179 | 100-109 |
| Grade 3: Severe | ≥ 180 | ≥ 110 |
| Emergency | > 220 | > 140 |
On 1 November 2021, ambulatory blood pressure monitors were added to the Medicare Benefits Schedule under item number 11607. Certain patients may be eligible for a Medicare rebate.

Associate Professor Harry G Mond OAM
MD PhD FRACP FACC FCSANZ
Founder and Medical Director CardioScan Pty Ltd
Dr Harry Mond is an Associate Professor at both Melbourne and Monash Universities and has been
practicing as a Cardiologist in Melbourne since 1975. He is a pioneer in cardiac pacing with
extensive experience in pacemaker implantation and follow-up. Dr Mond is currently involved in ECG
teaching and has completed a textbook on the subject.
For further information on how to order cardiac testing and patient eligibility criteria, please visit our Cardiac Services page.
If you enjoyed this article, subscribe to our electronic Pathology Focus newsletter.
Subscribe Today!References
- National Heart Foundation of Australia. Guideline for the diagnosis and management of hypertension in adults - 2016. Melbourne: National Heart Foundation of Australia 2016.
For more information on Ambulatory Electrocardiographic Monitoring, see Associate Professor Harry G Mond’s article ‘The Spectrum of Ambulatory Electrocardiographic Monitoring’ published in Heart, Lung and Circulation (2017) 26, 1160–1174.