The overlooked STI
By Dr Sudha Pottumarthy-Boddu
Published November 2025
Trichomoniasis is the most common curable, non-viral sexually transmitted infection (STI) worldwide. It is caused by the single-celled protozoan parasite Trichomonas vaginalis (TV). In 2020, the World Health Organization (WHO) estimated 156 million new cases globally among individuals aged 15 to 49 years.
Despite its prevalence, the true incidence remains unknown, as trichomoniasis is not a notifiable disease, except in the Northern Territory, and screening criteria are undefined. It has also been referred to as “the neglected STI” due to limited knowledge of its sequelae and associated costs.
Symptoms of trichomoniasis
- 70 to 80% of individuals experience minimal or no genital symptoms
- Men may present with urethritis, epididymitis or prostatitis
- Women may present with vaginal discharge, which can be profuse, malodorous or yellow-green
- In women with HIV, trichomoniasis is associated with an increased risk of pelvic inflammatory disease (PID)
Trichomonas vaginalis is associated with significant reproductive morbidity, including increased risk of preterm birth, premature rupture of membranes and small-forgestational age infants. Infection is also associated with a 1.5-fold increased risk of HIV acquisition.
Diagnosis
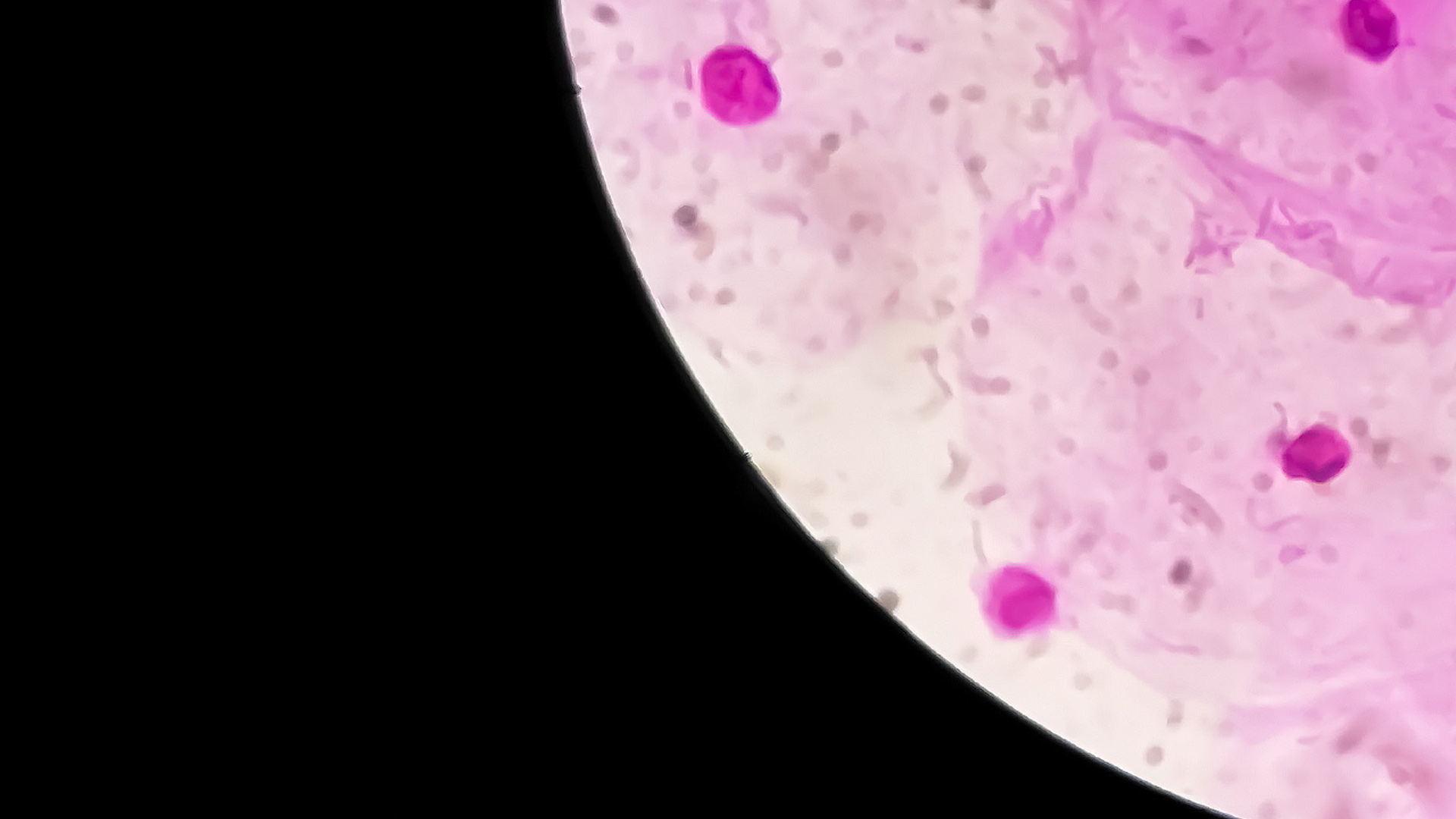
Wet-mount microscopy is an inexpensive point-of-care (POC) test used to diagnose Trichomonas vaginalis infection. However, its sensitivity is poor (≤ 66%) and declines rapidly to 20% within one hour of sample collection. Culture, with a sensitivity of 63-75%, may be used in conjunction with wet-mount microscopy to improve performance. However, it is labour intensive and can delay diagnosis by up to 7 days.
Nucleic Acid Amplification Tests (NAATs) provide a rapid and reproducible method for accurate diagnosis, with sensitivity and specificity > 95% (95.2–100%) compared to wet mount and culture. A recent study from the Melbourne Sexual Health Clinic reported a statistically significant 21% increase in Trichomonas vaginalis cases from 2011 to 2019, partly attributable to the shift from culture to NAAT. The diagnostic improvement with molecular methods has been widely recognised.
Treatment
- Recommended: Metronidazole 400 mg orally with food, 12-hourly for 7 days.
- Alternative: Metronidazole 2 g orally with food, single dose (less effective).
- Avoid alcohol during treatment and for 24 hours after the last dose.
- Advise no sexual contact for 7 days after starting treatment, or until symptoms have resolved and the course is completed, whichever is later.
- Recommend treatment for the current sexual partner.
- Further guidance available at sti.guidelines.org.au.
Test of cure
Not recommended unless symptoms persist.
If you enjoyed this article, subscribe to our electronic Pathology Focus newsletter.
How to Order Trichomonas vaginalis Testing
T. vaginalis PCR or Trichomonas PCR
A high vaginal or endocervical swab.
First-pass urine.
A dedicated red-top dry swab or Aptima Unisex Swab kit.
If routine vaginal bacterial culture is also required (MC&S), please provide a blue-top gel swab as well.
Click here to view the current NSW swab guide.
A high vaginal swab or urethral swab is required.
Use an orange dry swab for Trichomonas PCR testing, along with a blue gel swab for Microculture and Sensitivity.
Testing for Trichomonas PCR is also available on urine samples.
Bulk-billed, subject to Medicare eligibility criteria.
References
Trichomoniasis - STI treatment guidelines (2022). Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/std/treatment-guidelines/trichomoniasis.htm (Accessed: 04 June 2025).
Trichomoniasis. World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/trichomoniasis (Accessed: 04 June 2025).
Abraham, E. et al. (2022). ‘Positivity and risk factors for Trichomonas vaginalis among women attending a sexual health clinic in Melbourne, 2006 to 2019’, Sexually Transmitted Diseases, 49(11), pp. 762–768. doi:10.1097/ olq.0000000000001690.
Australian STI Management Guidelines. Available at: https://sti.guidelines.org.au/ (Accessed: 01 October 2025).