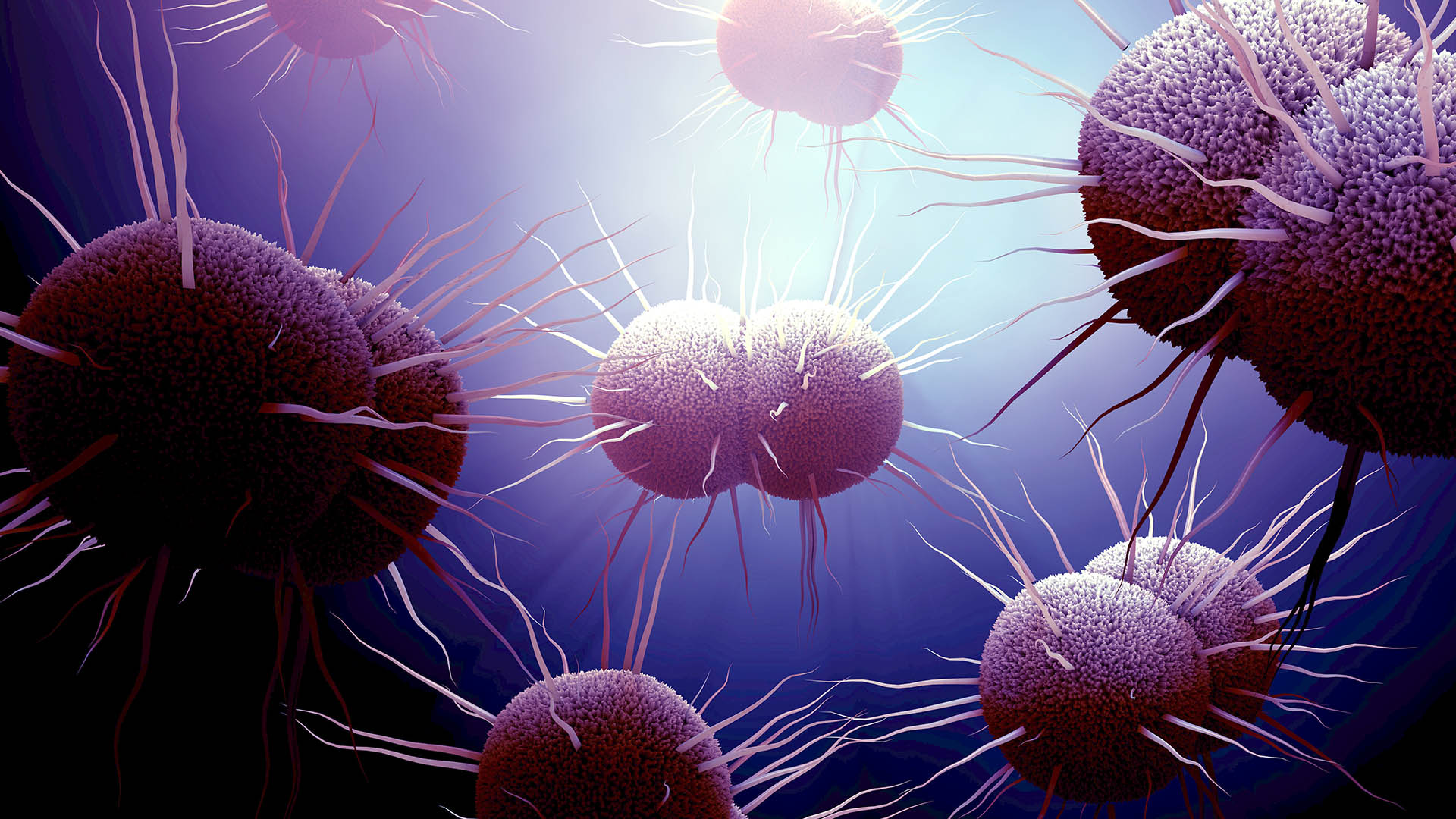
The bacterium Neisseria gonorrhoeae causes a disease spectrum very similar to that of chlamydia. In up to 3% of patients, bacteraemic (bloodstream) spread can result in disseminated gonorrhoea with presentations of septic arthritis, polyarthralgias or dermatitis. There was a concerning 16% increase in gonococcal infection notifications in Australia in 2023 (40,404) compared to 34,745 in 2019.
-
Symptoms
-
Treatment
-
Test of Cure
-
How to Order Gonorrhoea Testing
Request Form Instructions:Complete the Clinical Labs general pathology request form, listing gonorrhoea and any other required STIs.
If all recommended STIs for asymptomatic screening are required (gonorrhoea, chlamydia, syphilis, HIV, Hepatitis B and Hepatitis C), write “STI Screen” in the Clinical Notes.
Specimen Details:Urethral swabs, first-pass urine (FPU) and vaginal/endocervical swabs. Note: Vaginal/endocervical swabs are more sensitive than FPU samples in female patients.
Additionally, for Men Who Have Sex with Men (MSM): - Collect anorectal and pharyngeal swabs, even if patient is asymptomatic at these sites. - Collect an additional penile urethral swab for culture if discharge is present or before antibiotics.
If patient has symptoms, collect a clinician-collected endocervical swab. Swabs should be collected for culture to enable resistance testing prior to treatment.
Serology for HIV, syphilis, Hepatitis B and Hepatitis C if these tests are also required.
Test Cost:Bulk-billed, subject to Medicare eligibility criteria.